WHO reported Middle East respiratory syndrome coronavirus outbreak continues
On Dec. 24, 2025, the World Health Organization (WHO) reported that since the beginning of 2025 and as of 21 December 2025, a total of 19 cases of Middle East respiratory syndrome coronavirus (MERS- CoV), including four deaths have been reported to WHO globally.
Of the 19 cases, 17 were reported by the Kingdom of Saudi Arabia (KSA), and two were reported from France. Between 4 June and 21 December 2025, the Ministry of Health (MoH) of KSA reported a total of seven cases of MERS-CoV infection, including two deaths. In addition, at the beginning of December 2025, the National IHR Focal Point (IHR NFP) for France also reported two MERS-CoV travel – associated cases; involving individuals with recent travel to countries in the Arabian Peninsula.
The notification of these latest cases does not change the overall risk assessment, which remains moderate at both the global and regional levels. These cases show that the virus continues to pose a threat in countries where it is circulating in dromedary camels, with regular spillover into the human population. WHO recommends implementation of targeted infection, prevention and control (IPC) measures to prevent the spread of health care-associated infections of MERS-CoV and onward human transmission.
Since the first report of MERS-CoV in the KSA and Jordan in 2012, a total 2635 laboratory-confirmed cases of MERS-CoV infection, with 964 associated deaths (Case Fatality Ratio (CFR) of 37%), have been reported to WHO from 27 countries, across all six WHO regions.
Middle East respiratory syndrome (MERS) is a respiratory illness caused by a coronavirus (MERS-CoV). The case fatality ratio (CFR) among confirmed cases is around 37%. The CFR is calculated based solely on laboratory-confirmed infections and may overestimate the actual mortality rate since milder cases often go undetected or unreported.
Humans can contract MERS-CoV through multiple transmission pathways; the primary route being through direct or indirect contact with dromedary camels, which serve as the virus’s natural host and primary zoonotic reservoir. Additionally, human-to-human transmission can occur via infectious respiratory particles primarily in close-contact situations and can also occur through direct or indirect contact; this is especially prominent in health-care settings. Human-to-human transmission of the virus has occurred in health care facilities in several countries, including transmission from patients to health care providers and transmission between patients before MERS-CoV was diagnosed. It is not always possible to identify patients with MERS‐CoV early or without testing because symptoms and other clinical features may be non‐specific. Outside these environments, there has been limited documented human-to-human transmission.
MERS can present with no symptoms (asymptomatic), mild symptoms (including mild respiratory issues), or severe illness leading to acute respiratory distress and death. Common symptoms include fever, cough, and breathing difficulties, with pneumonia frequently observed, though not always present. Some patients also experience gastrointestinal symptoms such as diarrhoea. Severe cases may require intensive care, including mechanical ventilation. Those at higher risk of severe outcomes include older adults, individuals with weakened immune systems, and those with chronic conditions like diabetes, kidney disease, cancer, or lung disorders.
Tags:
Source: World Health Organization
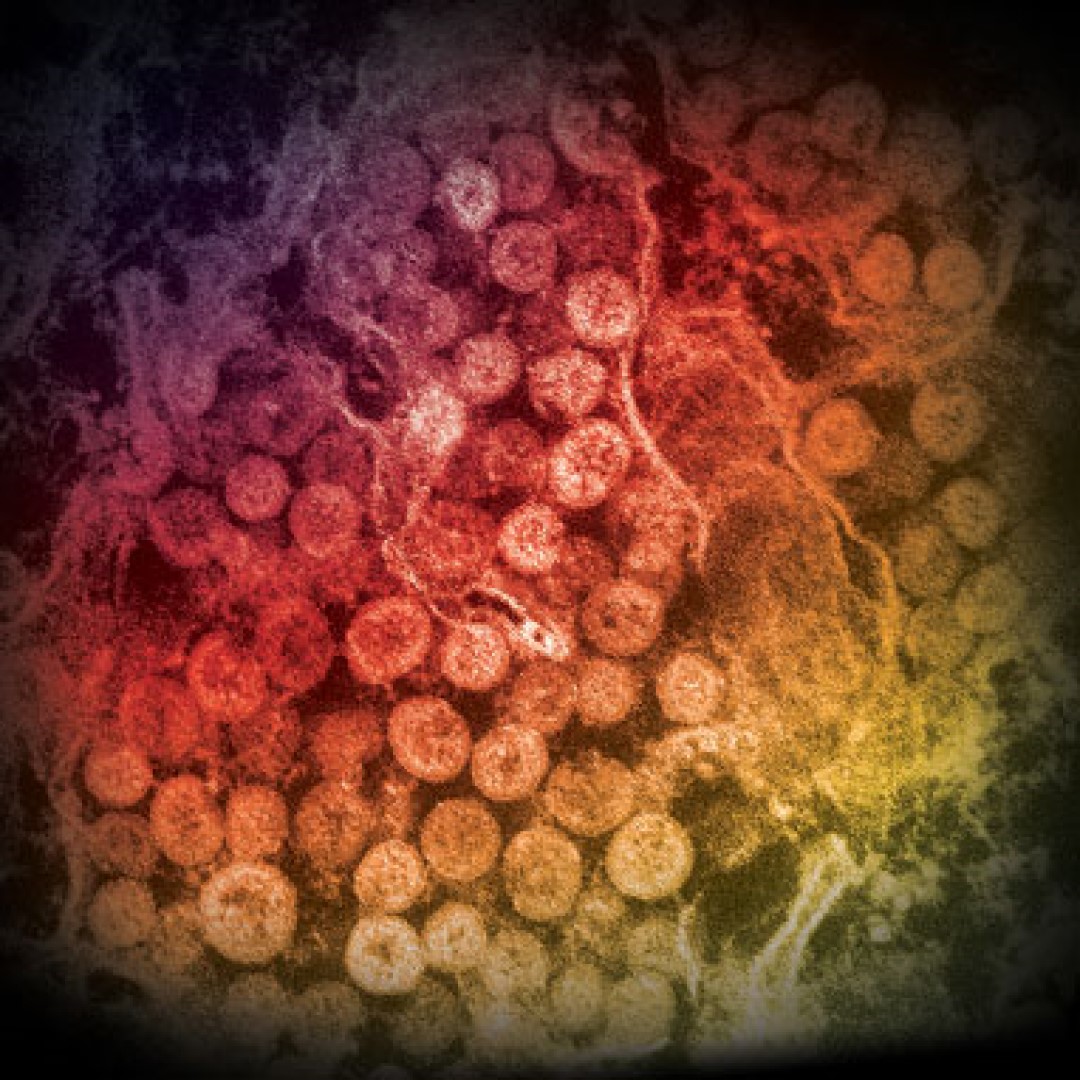
Credit: Image: An electron micrograph of a thin section of MERS-CoV, showing the spherical particles within the cytoplasm of an infected cell. Courtesy: Cynthia Goldsmith/Azaibi Tamin, U.S. Centers for Disease Control and Prevention.
