new antibody test only takes 10 minutes, no blood draw necessary
On Nov. 20, 2025, an interdisciplinary research team at the University of Pittsburgh has developed wearable biosensors that can detect antibodies associated with infectious pathogens such as SARS-CoV-2 and influenza viruses. The sensors are orders of magnitude more sensitive than existing tests, use only a half volt of electricity and can return results in just 10 minutes.
Unlike a traditional antibody screen that requires blood drawing, time and resource-inefficient laboratory tests, Star’s sensors detect antibodies in the interstitial fluid, a liquid surrounding human skin cells that contains many of the same proteins found in blood.
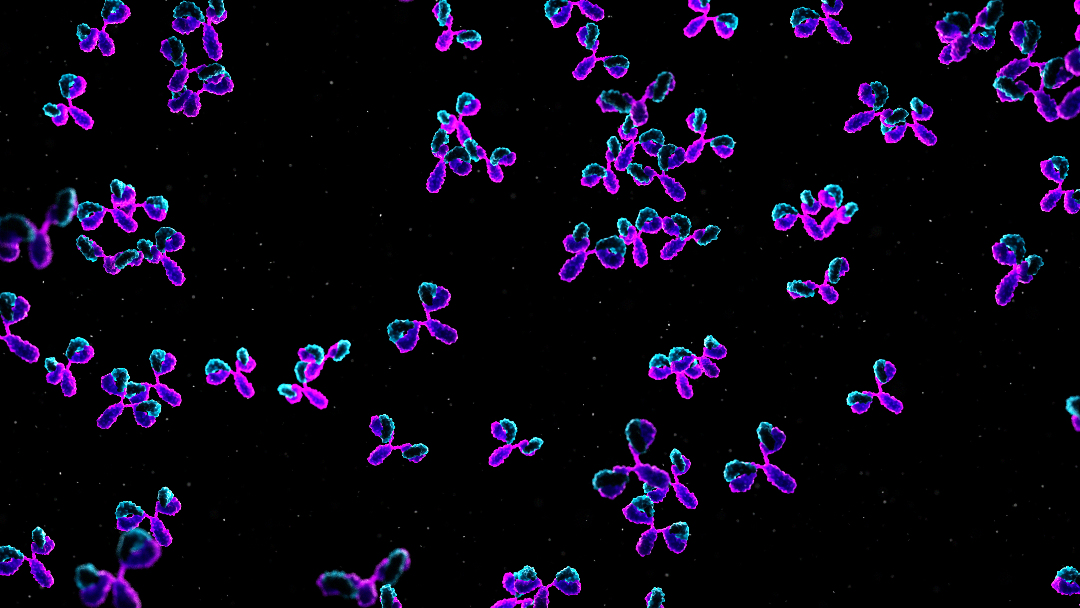
People’s immune systems are alerted to viral infections via viral antigens, molecules on the surface of the virus. To fight the intruder, the body releases antibodies, proteins designed to fight that specific virus. Over time, those antibodies fade.
In practice, people’s immune systems behave differently. After receiving a vaccine, which exposes the immune system to target antigens, one person may continue to produce antibodies for longer than another. Therefore, a booster might not benefit the first person but could be necessary to ensure the second person can fight off infection. The clearest way to know is to take an antibody test.
The chemistry team, including first author Amir Amiri, a graduate student in Star’s lab, designed two sensors — one to detect SARS-CoV-2-specific antibodies, which is responsible for COVID-19, and another to detect H1N1-specific antibodies, responsible for influenza A — by using the virus’ antigens as a lure and attaching them to carbon nanotubes, which are 100,000 times smaller than a human hair and have high electrical conductivity. An H1N1 antibody, for example, will quickly and tightly bind to a H1N1 antigen, indicating its presence by altering the electrical properties of the nanotubes.
Testing by a team in Pitt Medicine’s Department of Dermatology found Star’s sensors are nine orders of magnitude more sensitive than tests more commonly used in clinical labs, such as ELISA. “That means they can cover both trace amounts of antibodies and clinically relevant concentrations,” Star said.
Because of its high selectivity thanks to the use of antigens and superior sensitivity, there are a host of potential applications for Star’s biosensor platform. Paired with a microneedle array, it could prove to be a marked improvement over current biosensing methods used in the clinic. Their research was published in the journal Analytical Chemistry.
Tags:
Source: University of Pittsburgh
Credit:
