Stem cell engineering breakthrough paves way for next-generation living drugs
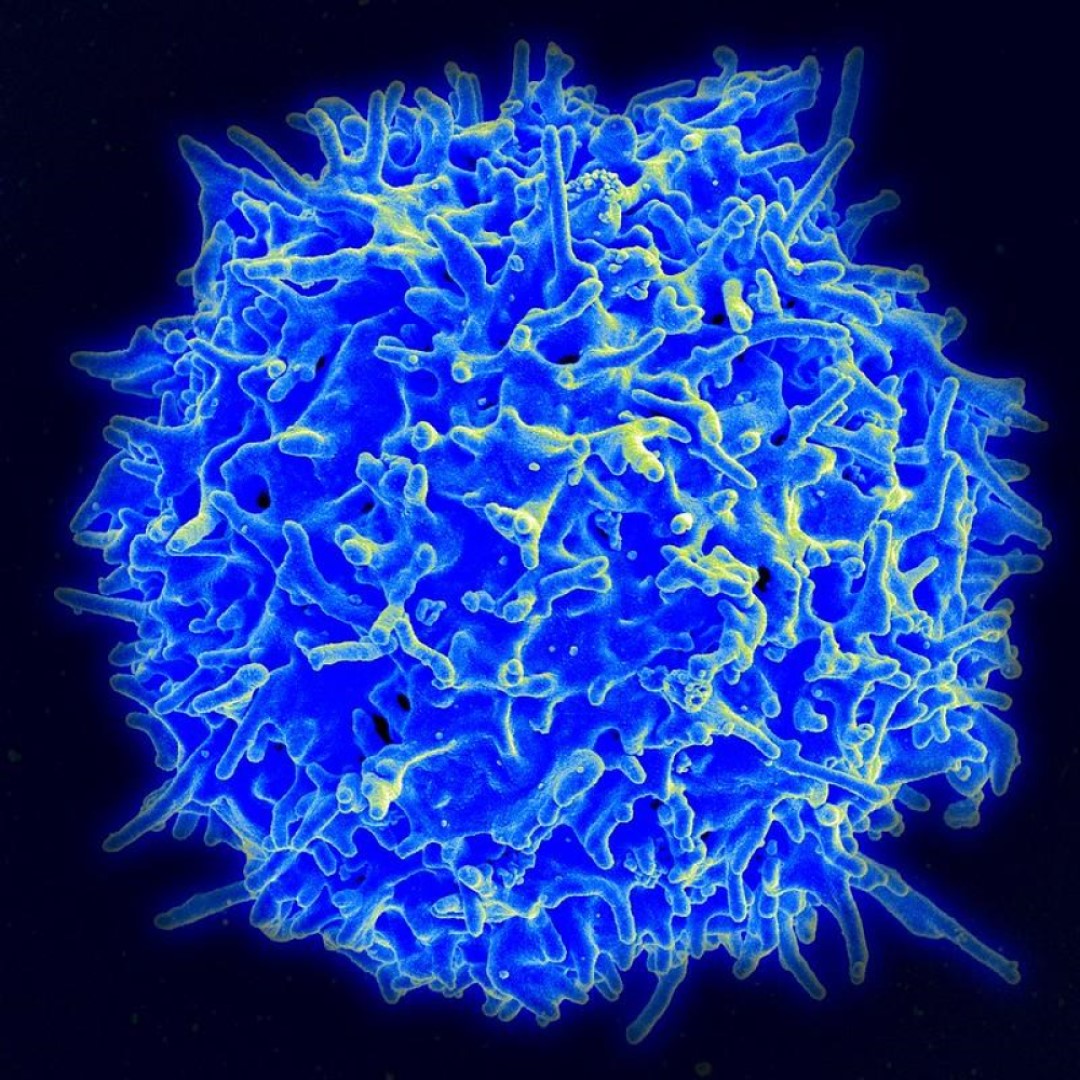
On Jan. 8, 2026, for the first time, researchers at the University of British Columbia have demonstrated how to reliably produce an important type of human immune cell—known as helper T cells—from stem cells in a controlled laboratory setting.
The findings, published in Cell Stem Cell, overcome a major hurdle that has limited the development, affordability and large-scale manufacturing of cell therapies. The discovery could pave the way for more accessible and effective off-the-shelf treatments for a wide range of conditions like cancer, infectious diseases, autoimmune disorders and more.
In recent years, engineered cell therapies, such as CAR-T treatments for cancer, have delivered dramatic and lifesaving results for patients with otherwise untreatable disease. These therapies work by reprogramming human immune cells to recognize and attack illness, essentially turning the cells into ‘living drugs’.
Despite their tremendous promise, cell therapies remain expensive, complex to produce and inaccessible to many patients worldwide. One major reason is that most current treatments are made from a patient’s own immune cells, requiring weeks of customized manufacturing for each patient.
In the new study, the UBC researchers were able to solve this long-standing challenge—adjusting key biological signals during cell development to precisely control whether stem cells developed into either helper or killer T cells. The team discovered that a developmental signal called Notch plays a critical but time-sensitive role. While Notch is needed early in immune cell development, if the signal remains active for too long, it prevents helper T cells from forming.
Importantly, the researchers demonstrated that the lab-grown helper T cells didn’t just resemble real immune cells—they behaved like them. The cells showed markers of healthy mature cells, carried a diverse range of immune receptors and could specialize into subtypes that play distinct roles in immunity.
The researchers say the ability to generate both helper and killer T cells—and to control the balance between them—will significantly improve the efficacy of stem cell-grown immune therapies in the future.
Tags:
Source: University of Bristish Columbia
Credit: